Table of Content
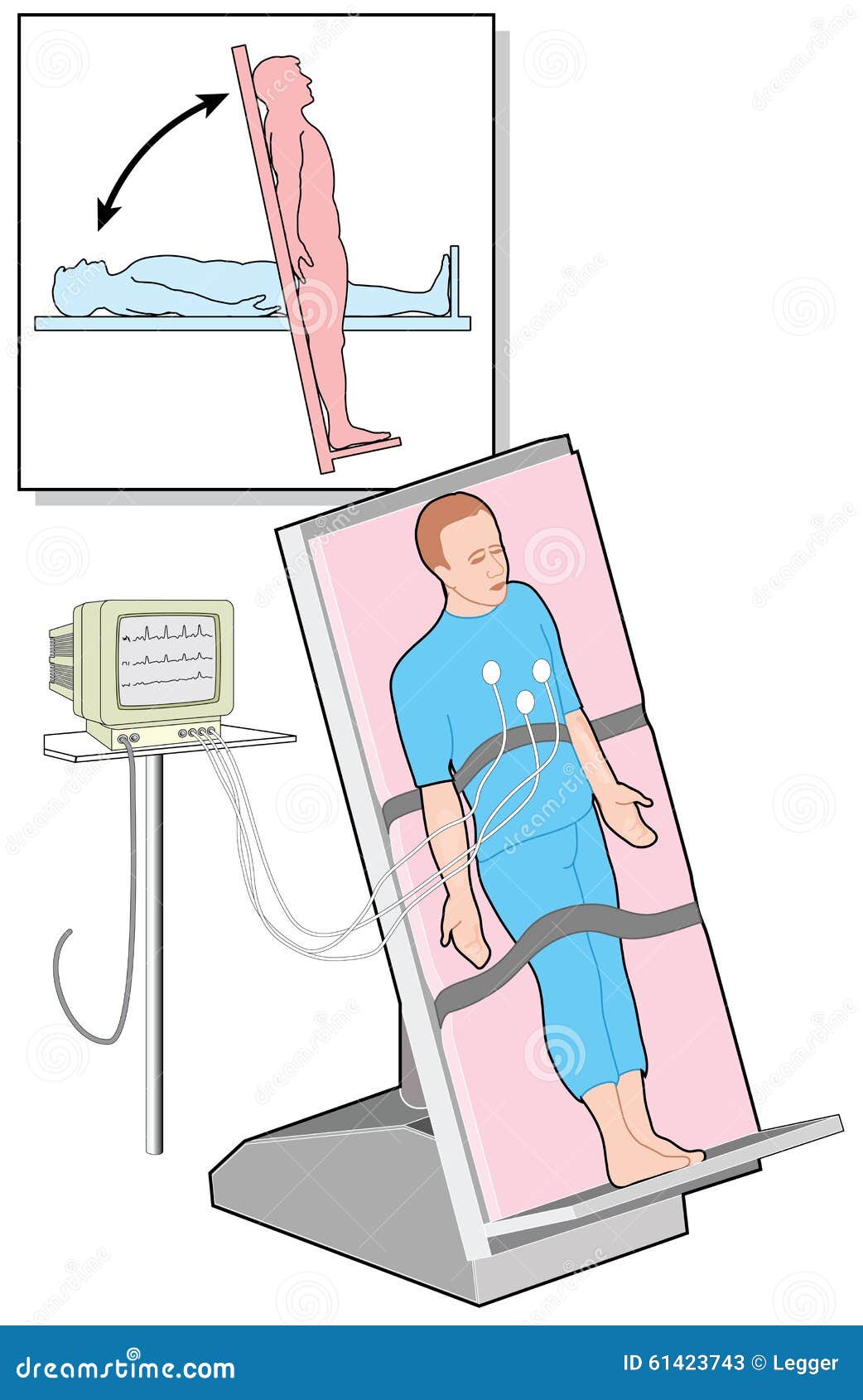
A tilt table test involves strapping a person to a table and moving it from a lying position to upright. This can help doctors identify the underlying cause of syncope. The change from lying down to upright may lead to an atypical response of the nervous and circulatory systems, resulting in a decrease in blood pressure. Doctors will move on to further testing if a tilt table test is positive. Several conditions can cause orthostatic hypotension and POTS. Doctors will combine this information with data from blood pressure and heart activity monitors.

The IV line is used to give you fluids and medicine, if needed. Small, sticky pads are put on your chest to monitor your heartbeat. PURE NormaLyte was created in partnership with Dysautonomia International for people with POTS. If you suspect you have POTS and you need relief now, you may want to consider giving NormaLyte a try. The Journal of Pediatric Medicine published a recent clinical trial surrounding the benefits or using an oral rehydration solution versus an IV. For me, it’s important to know the steps that will be taken long before I walk into my appointment so that I can psychologically prepare.
Frequently asked questions
Key personal information, including a family history of low blood pressure and major stresses or recent life changes. If blood pressure drops after eating, having small, low-carbohydrate meals might help. Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition. If this occurs, tell the team, who will then likely move the table so that you can lie down. They may administer treatment to reverse your symptoms and physiological changes if necessary.
While in this position, stay as still as possible and report signs and symptoms such as nausea, sweating, lightheadedness or irregular heartbeats. Wearing a Holter monitor, endless-loop recorder, or event recorder allows physicians to monitor your heart over days or weeks. You may be asked to keep a written journal of symptoms, or to push a button on the device when you faint or feel otherwise symptomatic.
What happens during a tilt table test for a child?
If you don’t have a change in your vital signs and still feel OK after the table has moved, you’ll progress to the second part of the test. However, people who’ve already had symptoms don’t need the second part of the test to show how their vital signs change when they move in position. You might not feel ill effects during the procedure, but you may experience symptoms like dizziness, feeling faint, or even fainting. A person with this syndrome can experience symptoms such as nausea, lightheadedness, and pale skin, followed by a loss of consciousness. If your blood pressure drops during this time, the nurse will lower the table and stop the test.

This effect is similar to that of strenuous physical activity. Doctors use tilt-table tests to find out why people feel faint or lightheaded or actually completely pass out. Places a blood pressure monitor or cuff on your finger, on your arm or on both to check your blood pressure during the test. If the heart rate is greater than 120 beats per minute at any point while standing, POTS might be indicated. Stand patient up still as possible for 2 minutes without leaning or moving. Take the pulse and blood pressure every two minutes while standing.
How will I feel during the test?
Knowing what to expect can be important for some. The test can also help distinguish syncope from other causes of loss of consciousness. Nonetheless, medical staff must have basic emergency training to perform a tilt test.
Do not eat or drink anything for at least four hours prior to your tilt table test. Check with your physician to determine if any of your medications should be avoided for the days leading up to your scheduled test. Make sure to bring all of your medications, as well as any herbal or dietary supplements and over-the-counter medications, to the test with you. The table will then be slowly tilted to a standing position, with your head up. Since you are strapped in, you will be supported in this position.
You will have a blood pressure cuff placed on your arm, as well as EKG leads placed on your chest. Your pulse and oxygen saturation will be monitored by a pulse oximeter, which is a small clip that is placed on the tip of your finger. Many people confuse a tilt table test with a stress test because both monitor heart function under modified conditions. However, a stress test is normally done for evaluation of chest pain, while a tilt table test is done for evaluation of fainting or dizziness.
Blood pressure decreases, causing dizziness or fainting during the test. If you don't faint or have other symptoms after 45 minutes, you might receive the drug isoproterenol through an IV line in your arm. The drug might prompt the reflex that causes you to faint.
Your doctor will talk to you about how to manage your condition. Oftentimes, increasing the amount of sodium you take in a day is the most recommended treatment plan. Your doctor will likely talk to you about the results of your test while you’re still in the office.
The major neurotransmitter of this system is norepinephrine, a catecholamine. Therefore, the catecholamine test can assess levels of sympathetic activity in a variety of situations. It is common to use an IV for blood draws to prevent distress at the time of the reading, as this would skew the results. Blood will be drawn after the patient has been horizontal for minutes, and then again after being tilted to a standing position. Treatment for orthostatic hypotension is directed at the cause rather than the low blood pressure itself.

No comments:
Post a Comment